Post Traumatic Residual
Orthopedic trauma surgery comprises some of the most complicated and difficult surgery encountered by the orthopedic surgeon in practice. A variety of techniques may be employed to stabilize injuries and the patient. Unfortunately, through no fault of the surgeon or patient, orthopedic complications may occur such as implant breakage, malunion and nonunion.
Post Traumatic Residuals produce abnormal alterations of the normal mechanics of the Musculoskeletal system. Depending on the original injury, they may occur anywhere and disrupt the normal function of any joint.
Certain injuries around the hip are predisposed to such problems. The femoral neck fracture was named “The Unsolved Fracture” precisely because of the common problems associated with this injury. Two of the more common problems encountered with this injury are avascular necrosis of the femoral head and nonunion of the femoral neck.
Proximal femoral deformities as the result of treatment of femoral fractures can be problematic, an angular malunion of the femur may cause problems with gait or healing of the fracture. Retained broken hardware may create challenges for subsequent reconstruction. These patients typically have hip pain, slight bowing of the leg, and shortening of the involved extremity. The end result is a mechanical disturbance which left untreated contributes to continued disability and pain in the patient’s life.
How does Osteotomy Surgery work?
In the young and active patient it is often preferable to correct the underlying deformities and address the healing problem in order to salvage the patient’s own hip. In a majority of cases, improvement of function and pain can be expected following correction of the underlying biomechanical problems. The workhorse technique for this problem is the intertrochanteric or proximal femoral osteotomy.
The surgical technique begins long before the scalpel is applied to skin. The procedure begins at the initial evaluation with a thorough history and physical. Documentation of history of infection or complication of surgery is important. Evaluation of the extremity and the neurovascular exam distal to the injury is important to anticipate problems which may occur. A liberal use of X-ray and or CT scan to document the deformity and it’s three dimensional problem is important.
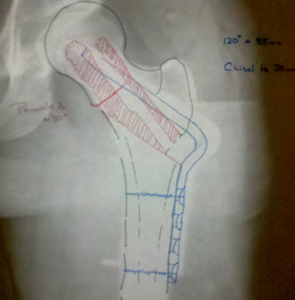
Preoperative planning is performed to document and predict the desired end result, the surgical tactic and the key kinetics of reduction and fixation. This is commonly done with a simple pen and paper prior to surgery.
Preoperative planning is a key to a successful surgery
Depending on the technical requirements of the surgery, the operation usually takes between two and five hours, with a blood loss ranging from 300 to 2,000 cc’s. A blood transfusion may be necessary but only as a last resort after using the cell saver.
At the time of surgery, implants from prior surgeries may have to be removed. It is common that parts of implants may have to be left in place as the difficulty in extraction outweighs the benefits of removal.
The goals of the procedure are to correct the underlying mechanical deformities, address limb length, and improve the biology of the bone to improve healing. When infection is present this may take one or more additional procedures to address and remove infected or nonviable tissues or bone.
How long is the recovery for Osteotomy surgery?
The usual hospital stay is 3 to 5 days and depends on how rapidly pain subsides and how the patient is progressing in physical therapy. After surgery, the patient will be monitored in either the recovery room. X-rays will be taken the day after surgery for a final assessment of the result.
Patients begin physical therapy while in the hospital improve hip motion and muscle function and to learn to use appropriate assistive devices such as crutches or a walker. The patient begins walking with crutches immediately, but weight bearing is usually restricted to 30 pounds on the operative side. Placing full weight on the operated side too early can cause the plate or screws to bend or break and the osteotomy to lose its position. Too vigorous exercise such as resistive exercise against weights can also cause failure. If failure occurs, re-operation may be necessary and the chance of complications and arthritis increase.
A team of medical specialists will care for the patient after surgery. Included among the team’s post-surgical priorities are pain management, preventing infection, and the prevention of deep vein thrombosis (blood clots in large veins), and pulmonary embolus (blood clots traveling through veins to the lungs).
After Discharge
The patient will go home after medical stability and physical therapy criteria are met. Before returning home the patient will be provided prescriptions for pain medications and an anticoagulant. Some degree of pain after discharge is natural which may increase or decrease on different days but the general trend should be toward decreasing pain. Some patients may sense an occasional “click” or “pop” in or around the hip these are natural and generally subside as time progresses. Numbness and a tingling sensation is common around the incision area. Follow-up outpatient visits are necessary to monitor progress by X-ray and physical examination. The first follow-up visit is usually scheduled about 2 weeks after surgery and the second at 6 weeks.
Once adequate healing of the injury has been established, the patient is allowed to be full weight bearing and work toward discontinuing use of the crutches. The patient may begin working with outpatient physical therapy at this time. Progress in walking depends on return of muscle strength. Subsequent follow-up visits are at 3 months, I year and 2 years after surgery and then at 2 year intervals.

